The COVID-19 pandemic has forever altered the healthcare industry. As a result of COVID-19, providers and insurance companies have been forced to change how they see patients and do business.
- Telehealth has emerged as a leading option to connect providers with their patients.
- The first quarter of 2020 saw the total number of telehealth visits increase by 50%.
- 66% of Medicare users report their usual providers offering telehealth.
- This is an increase of 18% from the previous year.
More Thank 1:4 Medicare Beneficiaries Had A Telehealth Visit Between Summer and Fall 2020
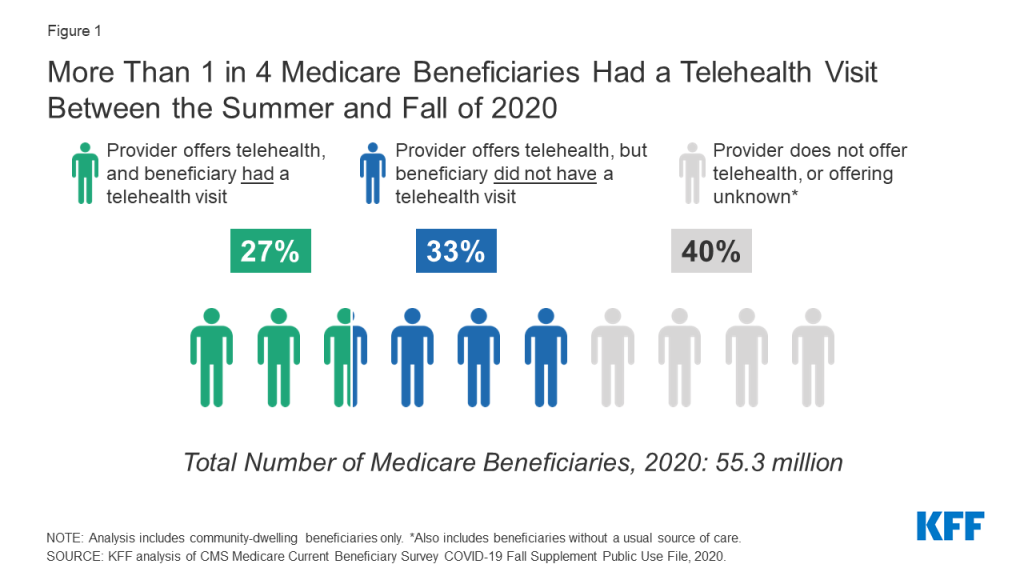
This uptick seems to be the trend for the foreseeable future. Until the public health emergency is declared to end, questions regarding billing Medicare for telehealth visits persist.
Medicare Reimbursement BEFORE COVID-19
Before COVID-19, traditional Medicare coverage of telehealth was limited to beneficiaries living in rural areas. Each telehealth visit had to originate from a clinic or doctor’s office. Beneficiaries living in urban areas were not eligible for these services. Medicare covers approximately 100 services, including psychotherapy and preventive health screening.
Before COVID-19, Medicare’s payment was the same whether the visit occurred in a facility setting. The payment rate was based on the lowest amount for a service delivered in person. This lower rate was used because it was reasoned that the provider’s expenses for a telehealth visit were lower than that of an in-person visit.
Medicare Reimbursement DURING COVID-19
When the federal government declared the COVID-19 outbreak a public health emergency in 2020, Congress and the Centers for Medicare & Medicaid Services expanded Medicare’s coverage of telehealth visits. During this time, beneficiaries can receive telehealth services in any geographic area. They can connect with providers from the comfort and safety of their own homes. They no longer must travel to a healthcare setting to meet with a professional. The list of permitted telehealth services expanded to include emergency visits and physical and occupational therapy. In addition, healthcare providers eligible to bill Medicare for professional services can also bill for telehealth services.
Medicare will pay telehealth providers as if each visit was an in-person visit. The payment rate depends on where providers perform the service. Consequently, a doctor in a non-facility setting will receive a higher payment than a doctor in a medical office. Medicare pays more for telehealth services now than it did before COVID-19. The new payment rates are slated to end when the public health emergency expires, but these rates are firmly in place now.
Additional Supporting Resources
The CMS.gov Medicare Telemedicine Heath Care Provider Fact Sheet can be found here.
Additional supportive material on Medicare and telehealth patient use and provider reimbursement information with data, metrics, and figures can be found here.
More information about Primoris Credentialing Network
Primoris Credentialing Network is a NCQA Credentialing Accredited specializing in credentialing and provider enrollment with 54+ health plan and network provider enrollment options. Primoris is a family member of Fifth Avenue Healthcare Services. Sister companies include 5ACVO (credentialing and primary source verification specialists) and Fifth Avenue Agency (MPLI and medical malpractice specialists).
Primoris Credentialing Network originally published this article here. For more information on Primoris Credentialing Network, please visit PrimorisCredentialingNetwork.com or Contact Us.